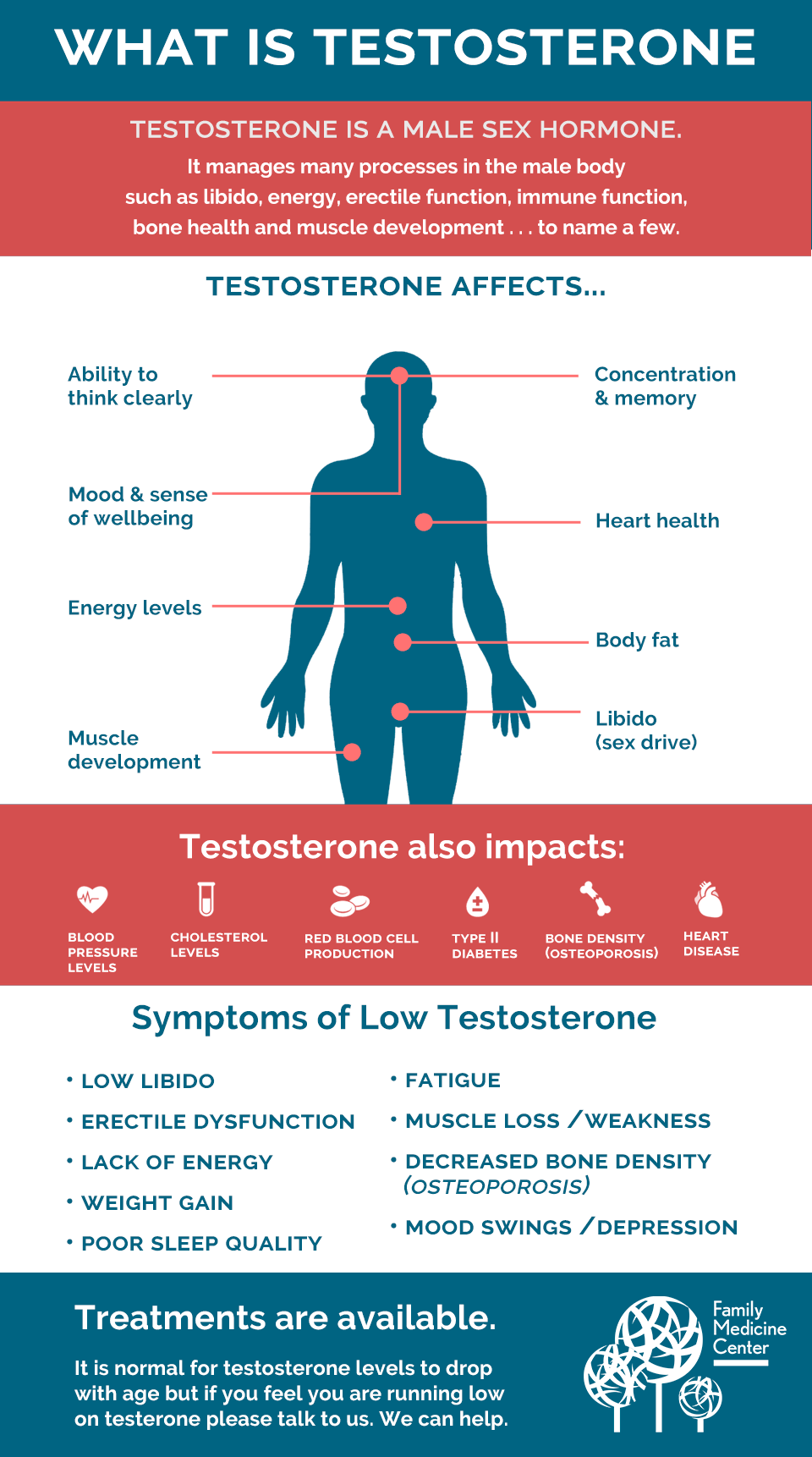
 The male hormone testosterone plays an important role in regulating sex drive, fat distribution, muscle mass, endurance, bone density, red blood cell production and sperm production, in addition to many other bodily functions. Testosterone levels generally fall as men age, but obesity is more influential in lowering testosterone levels than advancing age. Low testosterone is diagnosed when levels fall below 300 nanogrammes per deciliter.
The male hormone testosterone plays an important role in regulating sex drive, fat distribution, muscle mass, endurance, bone density, red blood cell production and sperm production, in addition to many other bodily functions. Testosterone levels generally fall as men age, but obesity is more influential in lowering testosterone levels than advancing age. Low testosterone is diagnosed when levels fall below 300 nanogrammes per deciliter.
The rate of obesity in the Bahamas has created a national healthcare crisis. Childhood obesity is an alarming health concern in our nation. It is estimated that approximately 40 percent of men in developed nations are obese. Obesity is defined as having a body mass index (BMI) greater than or equal to 30. Overweight individuals have a BMI greater than 25 but less than 30. The BMI is calculated by taking a person’s weight in kilogrammes and dividing it by their height in metres.
General and abdominal obesity are associated with an increased risk of premature mortality, but studies have shown that abdominal obesity could be a stronger risk factor for premature mortality than a high BMI.
Obesity and being overweight can lead to type 2 diabetes, insulin resistance and multiple comorbidities, including heart disease.
Cardiovascular disease, diabetes and kidney disease are some of the leading causes of obesity-related death and health complications.
Combating obesity is essential in reducing cardiovascular death in men in the Bahamas.
Healthy lifestyle changes and behavioural modifications related, for example, to implementing routine regular exercise and a healthy diet, are of paramount importance in combating obesity.
Hypogonadism, or low testosterone, is very common in obese men, with approximately 70 percent of obese men having low testosterone levels. There is a bidirectional link between testosterone deficiency and obesity. A vicious cycle exists whereby low testosterone contributes to the development and exacerbation of obesity and obesity can lead to low testosterone. Testosterone can be metabolised to oestrogen by fat cells, which will lower testosterone levels. Obesity also lowers testosterone by reducing the levels of the sex hormone binding globulin (SHBH), which is a protein that carries testosterone in the blood, so lower levels of SHBH leads to lower free testosterone levels.
Diet and behavioural modifications are the first step in achieving weight loss so that the vicious cycle of obesity and low testosterone can be addressed. Exercise and diet changes alone usually do not lead to sustained weight loss over a long period of time, particularly for men with low testosterone.
STUDY SUGGESTS OBESE MEN MAY BENEFIT FROM TESTOSTERONE THERAPY
Fifteen years of data was presented at the 2020 European and International Congress on Obesity, suggesting that testosterone therapy could be very useful in the management of some obese men, with low testosterone levels.
Dr Farid Saad, from the UAE’s Gulf Medical University School of Medicine, and colleagues investigated the relationship between obesity and testosterone for a period of over a decade. The research used a German registry tracking men with low testosterone over a 15-year period.
Professor Saad and research colleagues examined data involving 471 obese men who received long-term testosterone therapy and 276 obese men in a control group that did not receive testosterone therapy.
The testosterone therapy group of obese men were shown over a follow-up period of eight years to have lost 50 pounds on average. The obese men in the control group, who did not receive testosterone therapy, gained 13 pounds on average over the same follow-up period.
The important parameters of BMI, waist circumference and visceral fat measurements all improved in the testosterone receiving group when compared to the control group. The mortality rate was significantly lower in the testosterone group versus the control group; 7.6 percent compared to 32.3 percent.
A striking finding in this long-term scientific study, was that over 20 percent of men in the control group developed type 2 diabetes over the study period, whereas no men in the testosterone group developed diabetes over the same timeframe.
There were 76 morbidly obese men in the study, with 59 of these men having received testosterone replacement therapy and 17 of the morbidly obese men received no testosterone. The morbidly obese group lost an average of 66 pounds and the control group of morbidly obese men gained an average of 11 pounds over the study period.
In the prospective Massachusetts Male Aging Study (MMAS), shifting from non-obese to obese state in men led to a decline in testosterone equivalent to aging ten years. Testosterone therapy in obese men with testosterone deficiency and differing grades of obesity has shown in several large long term studies, to produce significant and sustained weight loss. The ideal testosterone preparation of testosterone replacement therapy for men wishing to preserve fertility, is the nasal spray. A side effect of most testosterone treatment preparations such as the intramuscular injection, the patch, gel or pellet therapy, is infertility as the testosterone treatment decreases sperm production by reduces levels of the hormone follicle stimulating hormone FSH, which is important in stimulating sperm production. In the majority of cases, the infertility caused by testosterone treatment is reversible.
The results of these long-term studies investigating the effects of testosterone therapy for obese men with low testosterone is very promising, but further broader scientific studies are needed before testosterone for obese low testosterone men could be validated.
• Dr Greggory Pinto is a board-certified Bahamian urologist and laparoscopic surgeon.
The Tribune
Published: December 28, 2021